#53 – No free lunch v. I’m in debt and hungry: The Debate on Industry and Education.
Episode host – Jonathan Sherbino.

Episode article
Hogan, S. O., Yamazaki, K., Jing, Y., Trock, B. J., Han, M., & Holmboe, E. (2023). Industry Payments Received by Residents During Training. JAMA network open, 6(10), e2337904.
In this episode of the PAPERs Podcast, the hosts delve into a hot topic in medical education: the relationship between industry and residency programs.
Jon presents a thought-provoking paper from JAMA that explores the financial connections between residents and the pharmaceutical industry, raising questions about ethics and the impact on professional identity. The team discusses whether guidelines and policies are needed to manage these interactions and reflects on the implications for medical training. Don’t miss this engaging debate on a critical issue in healthcare education.
Episode notes
Background
Where do you sit on the debate about residents and ties to industry/pharma? Ok, the easy headline is to take a posturing social justice warrior tone and resist the connection. Certainly, no one wants a health system where industry influence threatens the patient-physicians relationships. <cough, cough>. Recognizing that this debate can quickly ignite, incinerate, blow up a conversation between colleagues and friends (I’m struggling to find the correct framing of the metaphor), what should be the responsibility of a residency training program to limit industry connections to physicians-in-training? Should a paternalistic, sheltered approach be adopted? Should the approach be hands-off and guided by criteria/guidelines? What is the impact on professional identify? What does transition out of a sheltered training environment look like? What is the responsibility of faculty supervisors and mentors? Presuming underfunded programs are the norm, what are the resource implication of connections/no connections with industry?
Let’s take these “hypothetical” debates, add real data, and take a peek at the reality of residency education. Enter Hogan et al.
Purpose
From the authors:
“…using the [Open Payments Program] database, we can identify patterns of payments to residents that align with their specialty, gender, PD behavior, and sponsoring institutions.”
Methods
This is a cross-sectional, retrospective study using the Open Payments Program (OPP) database that tracks industry payment to US healthcare professionals. Reporting of payments to residents is NOT mandatory (likely reflecting an under estimation.)
In the academic year 2020-21, the 3 largest primary care (IM, FM, OBGYN) and surgical specialties (GSx, Ortho, Uro) were studied – residents, program directors, and programs.
A modified Poisson regression was used to determine the association of a resident-linked variable (dependent variable) to acceptance of payment (independent variable). The reference group (receiving the fewest payments) used for comparison was:
- Internal medicine
- female gender
- federally-owned institution (e.g., program type)
Results/Findings
Demographics:
- Approximately 66k residents (~47% female) with 30K IM trainees were included in study. Two-thirds of training programs were private, non-profit organizations.
Gross results:
- 27k payments made. ~22% (15K) of residents received USD$6.4M. 13% (9K) received $3.9M.
- ~40% of PDs (976) received $5.2M.
- Ortho received the most payments ($2.2M- residents, $4M-PDs). OBGYN the least ($68k -residents, $186k -PDs). Ortho had the highest proportion of accepting payment (40%) and IM the lowest (9%).
- Median payment to residents was $64 (21-194). Maximum payment was $50k. Median payment to PDs $119 (35-614). Maximum payment was $418k.
But… Types of Payment
- 90% food/drink
- 8% education
- 2% travel/lodging
- Grants (10 residents received grants of $10-50K)
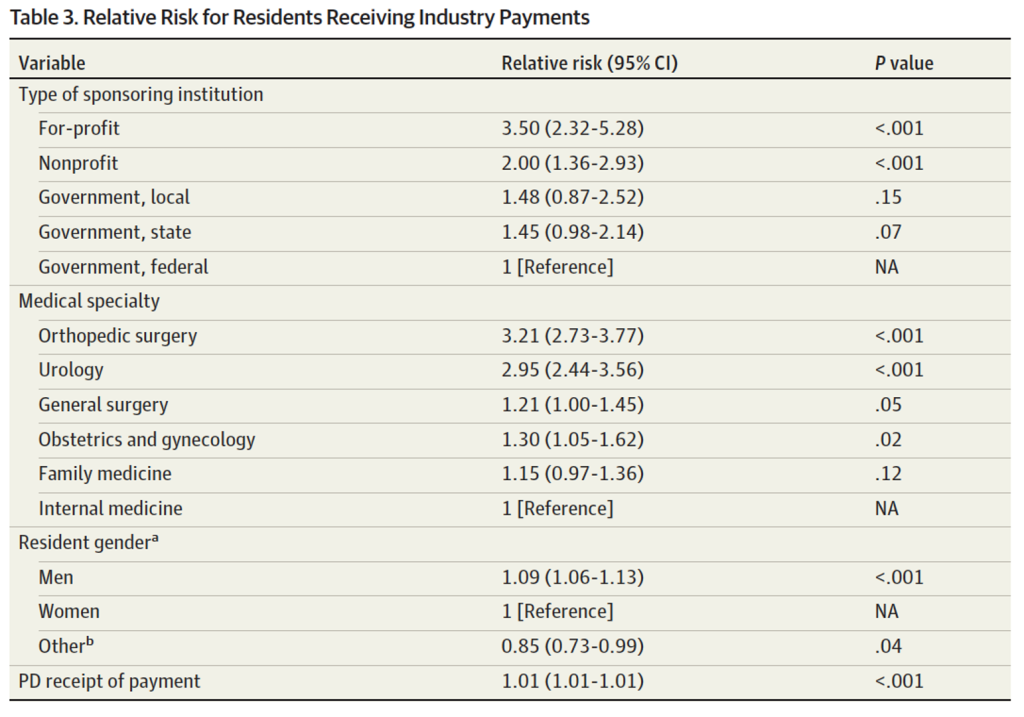
Relative risk for accepting payment:
Comments
From the authors:
“…approximately [22%] of residents were reported to have accepted industry payments in an academic year. That proportion could be an understatement because the available reporting is strictly voluntary. Specialty, PD behavior, and sponsoring institution control were significantly associated with residents accepting industry payments. Sponsored group meals appear to account for a large proportion of payments, suggesting that programs condone these trainee-industry interactions.”
0 comments